FDA takes steps to help reduce risks associated with surgical staplers
- Sanjay Trivedi
- Mar 10, 2019
- 4 min read
U.S. Food and Drug Administration issued a Letter to Health Care Providers to alert them that the agency is aware of an increasing number of medical device reports associated with the use of surgical staplers for internal use and implantable surgical staples—common devices used in many surgeries—and to provide updated recommendations to help reduce risks associated with their use. The letter also includes information about additional actions the agency is planning in the coming months to address the devices’ safety, including issuing a draft guidance with labeling recommendations for manufacturers and holding a public advisory committee meeting to discuss whether the current pathway for manufacturers to market surgical staplers for internal use is appropriate.
“As part of our public health mission, it is important that we communicate with the public when we become aware of issues stemming from the use, or misuse, of medical devices,” said William Maisel, M.D., M.P.H., chief medical officer in the FDA’s Center for Devices and Radiological Health. “As part of our Medical Device Safety Action Plan, we are committed to streamlining and modernizing how we implement post-market actions to address device safety issues to make our responses to risks more timely and effective. The agency’s analysis of adverse events associated with surgical staplers and implantable staples is ongoing, but we know these devices provide important benefits for patients undergoing surgery, so it’s important for us to continue to educate providers about the devices’ safety and risk. We are asking providers to be aware of the new information and implement the recommendations we’re outlining today to help improve the safe use of these devices. Improving the safety of surgical staplers and implantable staples is a top priority for the FDA, and we believe our forthcoming draft guidance to industry and planned advisory committee meeting will advance those efforts.”
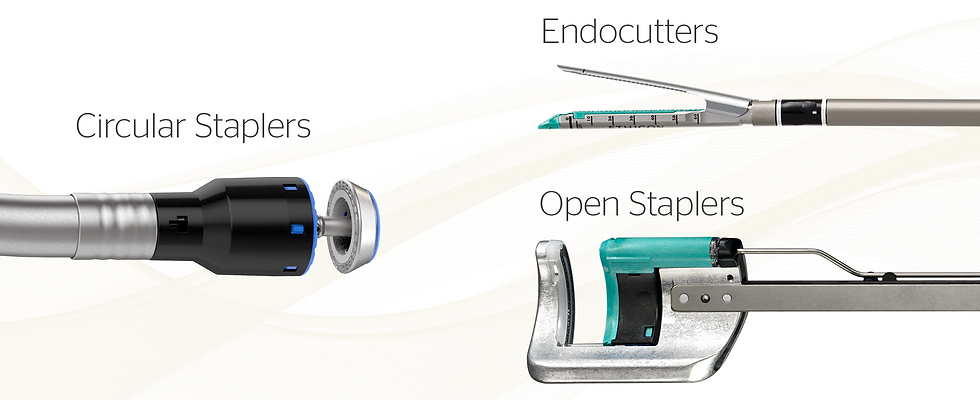
Surgical staplers and staples may be indicated for use in a wide range of surgical applications, including gastrointestinal, gynecologic, and thoracic surgeries to remove part of an organ, to cut through organs and tissues, and to create connections between structures. These devices facilitate surgical procedures and may shorten surgical procedure time compared to manual suturing. Currently, surgical staplers are regulated as Class I medical devices, which do not require a premarket submission to the FDA. Implantable surgical staples are classified as Class II medical devices and require premarket review before marketing.
The agency has issued previous communications about the risks involved with surgical staplers and implantable staples and has been conducting an ongoing assessment of medical device reports (MDRs) filed with the agency. The agency’s analysis shows that from January 1, 2011 to March 31, 2018, the FDA received more than 41,000 individual MDRs for surgical staplers and staples for internal use, including 366 deaths, more than 9,000 serious injuries, and more than 32,000 malfunctions. The FDA continues to evaluate the MDRs for these devices.
The most commonly reported problems in these adverse event reports include an opening of the staple line or malformation of staples, misfiring, difficulty in firing, failure of the stapler to fire the staple, and misapplied staples (e.g., user applying staples to the wrong tissue or applying staples of the wrong size to the tissue). Stapler and/or staple malfunctions or misuse may result in prolonged surgical procedures or unplanned, additional surgical interventions, which may lead to other complications such as bleeding, sepsis, tearing of internal tissues and organs, increased risk of cancer recurrence, and death.
In today’s communication, the FDA is reminding providers to review labeling instructions and indications for use for surgical staplers and implantable staples, such as choosing the appropriate staple size for the patient’s tissue type and thickness. The letter to health care providers also suggests considering alternative options if the patient’s tissues are swollen, prone to bleeding, or dead (necrotic). The FDA further provides recommendations on how to recognize and manage device malfunction.
For patients, it is important to understand that when used correctly, surgical staplers and staples can be beneficial surgical tools. These devices are regularly used in many types of surgical cases, and enable a surgeon to perform a less invasive operation, which may reduce postoperative pain and shorten recovery time. The types of adverse events observed with surgical staplers and staples may similarly occur with hand sewn alternatives. The purpose of the letter to health care providers is to remind them of the importance of appropriate selection and use of surgical staplers and staples to mitigate risk.
In addition to the letter to health care providers, the agency is taking steps to address the safety of these devices.
The FDA intends to issue a new draft guidance for public comment this year, which will describe proposed recommendations for manufacturers of surgical staplers and staples for internal use about information to include in their product labeling, which will help health care providers better understand the appropriate use and the risks of these products.
In light of the identified risks of surgical staplers, the agency also intends to hold a public meeting of the General and Plastic Surgery Devices Panel of its Medical Devices Advisory Committee this year to discuss whether the current pathway for manufacturers to market surgical staplers is appropriate. As part of the panel meeting, the FDA will present a comprehensive analysis of all the MDRs received for surgical staplers and staples for internal use, as well as other relevant information, and will seek panel input on whether reclassifying surgical staplers for internal use is appropriate. Reclassifying surgical staplers for internal use from Class I to Class II would allow the FDA to establish special controls, such as mandatory performance testing of various mechanical features, demonstration of usability and labeling comprehension (assessing user’s ability to properly select and use the device according to the labeling), and specific labeling elements supporting the safe use of the device.







Comments